
Andy McVittie talks us through elbow tendinopathies and the first steps in solving them in the context of the Coronavirus lockdown. For more information, visit Andy's website here.
It appears if we're not using lockdown to work out, hard, every day we're losers who will be weak and feeble when restrictions are lifted. As pointed out by Madeleine Crane you don't HAVE to. Live now, climb later!
What about using this time to tackle those long-term issues that dog many climbers?
This article is an accessible look at tendinopathies of the elbow and how to start treating them, with no equipment, during lockdown.
Tendinopathies are 'sticky' and painful. They hang around like a bad smell and are hard to get rid of. The vast majority of literature recommends protocols of 12 weeks plus, so maybe now is the time to stop using air freshener to cover up the smell and tackle its cause?
What's in a name?
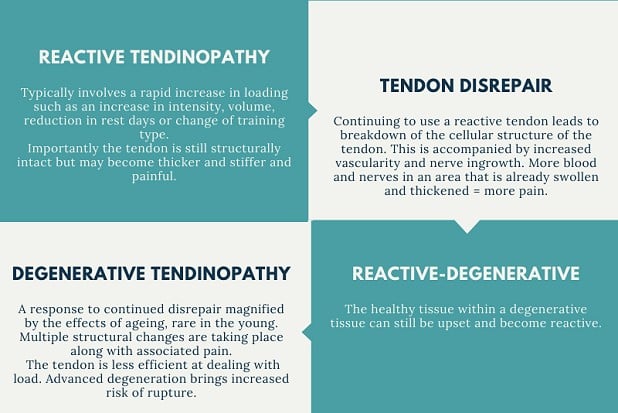
Rather than get bogged down in technicalities it's much easier to think of tendinopathy as a continuum: reactive tendinopathy, tendon disrepair and degenerative tendinopathy.
- Reactive Tendinopathy - Typically involves a rapid increase in loading or reduction in rest. Sound familiar? Have you just started using that fingerboard you put up 2 years ago but never used? Importantly at this point the tendon is still structurally intact but may become thicker, stiffer and painful.
- Tendon disrepair - Ignoring the niggle? Then say hello to disrepair. Breakdown of the cellular structure of the tendon is accompanied by increased vascularity and nerve ingrowth. More blood and nerves in an area that is already swollen and thickened = more pain.
- Degenerative Tendinopathy - The bane of us older weekend warriors. A response to continued disrepair magnified by the effects of ageing. Youth can still get this, it's just more common the older you get. Multiple structural changes are taking place. The tendon is less efficient at dealing with load. Advanced degeneration brings increased risk of rupture. Oh, and more pain.
A degenerative tendon can become reactive also. There is still healthy tissue within the tendon to react. A lovely double whammy. Yes, I mean more pain.
The treatment that follows is a good start no matter your place on the continuum.
Treatment
We need to improve the capacity of the tendon and muscle to manage the load you want it to handle without irritating it. Tendons won't adapt with rest and they don't like rapid change. Be patient.
So, with a big, broad brush I shall present what I have found to work for the majority with the 7 stages of elbow tendon rehab.
Rehabilitation stages
- Reduce pain
- Improve strength of the musculo-tendonous unit
- Build functional strength
- Increase power
- Develop the stretch shortening cycle (plyometrics)
- Sport specific training
- Maintenance of optimal tendon health
For now, we'll look at just 1 and 2 as that will take 8-12 weeks for most.
Stage 2 is where most stop rehab. The tendon becomes painless and they crack back on. Missing the next stages means it is very likely to re-occur and you've wasted your rehab effort.
1) Reduce pain
Don't stretch
But it feels so good! Tendons are subjected to normal tensile (pulling) forces and compressive (squashing) forces as they are pulled tight against the bones they travel over. Both flexor and extensor tendons can be affected by compression. This is a type of load which can irritate them when sensitive.
Isometric (static) exercises
Reduce training to manageable levels, or stop for a short while. Tendons don't really respond to rest, so one week max is fine.
Consider using your other hand for daily tasks like opening doors, carrying bags, brushing teeth etc. The more opportunity you can give it to recover the better.
Isometric exercises can be helpful to reduce pain and maintain tendon/muscle capacity. They can be done anywhere anytime. This stage may take a couple of weeks.
Not everyone needs this stage. If your pain feels manageable throughout the day and only flares up a bit after activity then progress to stage two. You can still use these exercises to help pain settle if you have a small flare up.
Play about with the position of the exercise so it makes your sore bit wake up, but not scream.
Highly irritable tendons may benefit from performing the exercise on both elbows at the same time with a shorter hold time and for fewer repetitions. Build from there.
See the summary sheet below for the exercise protocols.
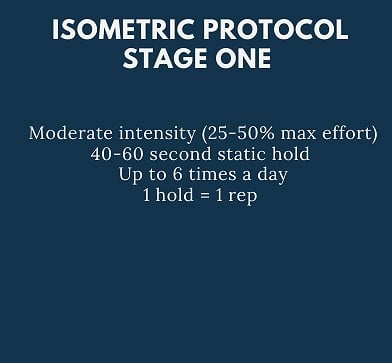
Keep a symptom diary of your progress using the sheet for stage 1 by using this PDF.
Use the scale below for reference:

When your daily total is 12 or less for 3 consecutive days you can move on to stage 2 if you feel ready. There is no harm in continuing a while longer.
Further measures
Use of pain killers is effective and ibuprofen is recommended in the reactive phase, as it reduces the process of water ingress into the tendon. However current advice needs to be borne in mind and consult your doctor before taking any medication.
Try heat as well/instead of painkillers. Ice treatment is not recommended anymore in an acute (reactive) phase.
2) Improve strength
Tendinopathy is likely to result in reduced muscle strength and function.
Progress to this stage once you're able to perform your daily life (not exercise) without your pain going above 3 on the scale. Don't provoke your pain above 5 by training or these exercises.
Keep a symptom diary of your progress using the stage 2 sheet here.
Muscles take 6-8 weeks to form long-lasting adaptations and tendons take 12 weeks+ to do the same. Be patient and consistent.
- The resistance you provide depends on the stage and severity of your condition. It is governed by you. Pain of no more than 5 out of 10 which settles back to baseline within 20 minutes.
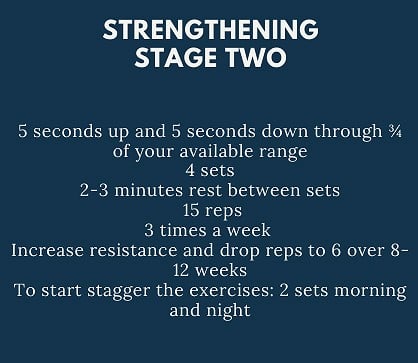
- Heavy Slow Repetitions (HSR) are my current favourite for this stage. See the summary sheet below for the protocols:
Tennis elbow
The most common culprit involves the wrist extensor on the thumb side and causes pain on the outside of the elbow. Opening jars and gripping anything hurts.
1) Hold the stick by the handle in your affected hand. Grip with your thumb on the same side as your knuckles.
2) Place the inside of your arm flat on a table top, arm fully extended. The edge of the table should be touching your armpit.
3) With the stick horizontal (9 o'clock if it's your right arm) apply resistance with your other hand to the top and lift the stick to (11 o'clock)
4) Use your free hand to provide resistance back down to 9 o'clock position
5) Re-test at different angles (elbow straight, 45, 90 and 135 degrees)
6) find the angle that reproduces your pain and that is the position you use for the exercise
Golfer's elbow
Commonly involves the wrist flexor on the little finger side and one of the muscles responsible for turning your hand to face palm down. So this gets two exercises. It causes pain on the inside of your elbow. If washing your hair hurts your elbows you've probably got this.
1) Hold the stick horizontally in your affected hand, palm up, with thumb on the same side as your knuckles.
2) Place your arm (still palm up) on a firm surface with your wrist being well clear of the table edge. Your elbow should be fully straight.
3) Lean your body over your arm to lift the painful area a couple of centimetres off the surface.
4) Apply pressure to the top of the stick with your unaffected hand, on the same side as your little finger.
5) Raise the wrist up to nearly full flexion.
6) Lower back down until near full extension still applying resistance with the unaffected hand.
7) Re-test at different angles (elbow straight, 45, 90 and 135 degrees).
8) Find the angle that reproduces your pain. That is the position you use for the exercise.
The same applies for the second exercise, but don't raise the inside of your elbow off the surface. This time apply pressure as you move the stick from 3 o'clock to 1 o'clock. The opposite of the tennis elbow exercise and shown in the picture below:
Have a rest for a few days around week 4 and 8. Don't forget to keep making sure that the angle you're working at is hitting 'the spot' by adjusting your elbow angle.
How do I know if I've done too much?
This is tricky, but well suited to providing your own resistance with your other hand. If you feel you should be able to complete 10 reps at weight X you may push on too far. By providing your own resistance you can micro-adjust every rep to stay in that sweet spot and account for lowering a weight requiring a higher resistance than raising it.
Feel free to tweak this program. It's a fine balance between stimulation and aggravation that you are in control of.
If you're not eliciting 'your pain' then increase the weight and drop the reps.
If your pain becomes too uncomfortable during exercise, if it is still hurting at the same level 20-30 minutes after exercise, or if it flares up the next day that was too much.
Tendons have an annoying habit of feeling OK during the session, but then hurting the next morning. Keep the simple diary noted above so you can see progress and adjust accordingly.
Training can still go on. Don't train on 'elbow day'.
Top tip! If your tendon feels a little bit irritable in the mornings but better in the evenings then do your exercises in the evening.
Top tip 2! Being able to do more with the same amount of pain is progress. If you feel your pain has stagnated don't feel you're not improving. It's likely to feel a little niggled as you're exercising it.
If you would like further info regarding sources or the protocols then please get in touch through my website.
To download the full information sheets on elbow tendinopathies, head to this page.
This advice is not meant to replace assessment and treatment from a trained health professional. Tendinopathy rehab is complex and can be challenging. There are MANY differential diagnoses present as tendinopathy. I hope to provide general guidance and education with this article, but I would recommend seeking a physio for professional advice specific to your case. Tendinopathy is recognised as benefiting more than most conditions from individualised treatment. I am attempting to provide enough information to allow you to vary your own treatment within parameters.
Remote assessment and treatment is available from providers at present and has been shown to be very effective in previous long-term studies within healthcare.
As a climber, climbing coach and physiotherapist (who has also done a fair bit of running and cycling), Andy is ideally placed to provide clarity and direction to your return to climbing and outdoor sports.
A life long climber, who started coaching 13 years ago, he has coached on Spanish performance improvement holidays, sport climbing, competition climbing and helped people achieve everything from ascents of El Cap to their first V11. More recently he founded a youth competition climbing squad https://processcoaching.me/ with his business partner Ellie.
Whilst his focus in coaching is technique based, his passion in physiotherapy is education, strengthening and a detailed, fully supported, return to sport. This background enables a unique, blended, treatment approach, with an in-depth knowledge of all aspects of how climbing impacts the body.
2020 was going to mark his proper return to sport climbing with an aim of 7c onsight. Fingers crossed it may still happen…..
- GEAR NEWS: The Self Rehabbed Climber, by Andrew McVittie 5 Dec, 2022
- SKILLS: Core Training for Climbing 15 Feb, 2022
- SKILLS: Improving Heel Hook Ability and Reducing Injury Risk 22 Apr, 2021
- SKILLS: Elbow Tendinopathy - The Boomerang Condition 2 Sep, 2020




























Comments
From my experience, long term Tendinopathy (more than 12 months) nothing really works other than heavy mechanical load, isometrically or eccentrically, however isometrically you can exert the highest force and therefore work the whole of the tendon and get to the "damaged" part. Otherwise you just exercise the good part of the tendon, so basically a waste of time, at least it was for me. And I say "damaged" between brackets because it's not clear whether, say after 6/12 months of pain, the tendon is injured, scarred, it has gaps in the collagen structured and therefore making it weak or the pain is a nerve response (apparently the tendon has nerves on the outer sheath, according to Dr. Hakan Alfredson). I recommend the first thing to do if you think you have a serious tendon issue is to get an ultrasound scan, ideally by two different surgeons, to see what really is going on. However, by talking to vast majority of people, most tendon issues to majority of people go away on their own, no matter what they do as rehab, just stopping doing what aggravate it in the first place.
Hi Ramon. There was so much i originally wrote that then got cut out, so it was still an article and not a dissertation. It's a huge subject. This is obviously a generalised approach, that's why i added at the end that the most effective treatment is an individualised one.
My emphasis (hopefully) is on patients finding the spot that recreates 'their pain' and working there. Changing the position after re-testing as mentioned. You're quite right on that point.
What often causes pain to reduce is indeed to reduce the aggravating factors. But the tendon will not repair itself effectively without structured strengthening and a graded return to the activity that upset it in the first place. Without this it will be susceptible to re-occurring at a similar level of activity in future. A recent patient had been able to continue climbing for ten years with golfers, as long as he stayed below a certain threshold. Small interventions were all that was needed to set him on the right track to symptom manage and truly grade his return back to where he wanted to be and now, happily, beyond.
Ultrasound does definitely have its place, but my preference is not to go down that route until after 6-12 weeks of conservative treatment. And not so i get all the appointments. A thorough screening of differential diagnoses (such as rheumatological conditions) and consideration of intrinsic factors should factor out the need for an ultrasound and a confident diagnosis of a tendinopathy and nothing sinister. A program, which is tweaked as you go along, is implemented considering their goals and current capacity. If there is no improvements after 6-12 weeks then yes further investigation is needed and ultrasound could be one of the options as part of a treatment review.
Whist is a great way to spend the lockdown
Yes of course the nature of the article has to be brief and to work for the majority and miss the more in-depth info. But my response was more about my experience with low loads which is what most articles online promote, and I thought there was a lack of mentioning the benefits of high mechanical loads and therefore that's why I commented, for the benefit of others who might ended up in many dead roads like myself.
Why I meant on my last line, poorly explained, was that from my experience talking to a lot of climbers and professionals is that there seems to be a wide range of (low-load) interventions (therabands, low weight eccentrics, supinations, therabars, arm-aids, Randalls stretch for golfers...) that climbers attribute to their success to recovery. However that might just be a combination of accepting that the elbow needs attention and the consequential awareness, stopping aggravating elements and some of the exercises (if they correctly prescribed as you say). But that can be hit and miss depending on what specialist you talk to. I've done protocols for up to 3 months that were a waste of money and time. I've also amassed a collection of useless contraptions in the process.
I'm not a professional by any measure, but I just have to disagree with you that an ultrasound at an early stage is not advised. I'd probably say it might not be necessary for the vast majority of cases, but for those that the condition can complicate it can be invaluable. I for one wished the first thing I did was get an ultrasound, it would have saved me so much time and money. In fact it wasn't until I got two different scans with the same diagnosis (one by Chris Myers and the other the Hakan Alfredson) that I actually got the right answers and now I do have a protocol (tendon density training) that I'm finally seeing some progress with.
This is by no means a criticism of your article, but I've taken the opportunity of this article to give a side-note based on my experience that the general advise doesn't always work for everyone.
And they are all very fair points Ramon. I didn’t take them as criticism and my response was just to explain why I hadn’t been able to write all I wanted.
I’m glad you got there in the end, even if it did take a long time for you.